Male to Female
gender reassignment surgery
Gender reassignment treatment has been demonstrated as the most effective treatment for patients affected by gender dysphoria.

Gender reassignment treatment (which includes psychotherapy, hormonal therapy and surgery) has been demonstrated as the most effective treatment for patients affected by gender dysphoria (or gender identity disorder), in which patients do not recognize their gender (sexual identity) as matching their genetic and sexual characteristics.
Gender dysphoria, also known as transgenderism or gender identity disorder (GID), is a condition in which a person feels a major mismatch between their biological sex and their gender identity. It is not a type of mental illness, although it was wrongly believed to be one in the past.
People with gender dysphoria can be treated with counselling, hormone therapy and sex change surgical procedures. Not every transgender individual requires or wishes to undergo sex change surgery. Some are treated with counselling only; others may get counselling and/or hormone therapy. But some trans people do end up going through sex change operations.
Sex change surgery is irreversible. Therefore (and obviously) anyone wishing to undergo a sex change operation from male to female should carefully consider that decision.
Sex change surgery is a series of complex surgical procedures (genital and nongenital) performed for the treatment of gender dysphoria. Male-to-female sex reassignment surgery involves reshaping the male genitals into a form with the appearance of, and as far as possible, the function of female genitalia.
Sex change surgery usually follows hormone therapy. It is necessary to have a letter from a psychiatrist before a physician begins hormone therapy.
A patient must be over 18 years and understand what hormones can and cannot do medically. It is also necessary to understand the social benefits and risks of hormone therapy. A minimum of three months of psychotherapy or a documented three-month real-life experience is necessary to be eligible for hormone therapy. MTF people should have stable mental health and demonstrate their ability to take hormones in a responsible manner to be started on harm one therapy by a physician.
For MTF's hormone therapy involves taking the female hormones oestrogen and progesterone as well as blocking agents for the male hormone testosteronetaken orally or by injection.It will be necessary during all stages of the transition, before, during and after the sex change surgeries. Hormone therapy in male to female transition is important because it helps change the physical appearance to resemble a woman more closely.
For some people, all the treatment they need to treat transgenderism is hormone therapy. Because hormones affect the way they feel, they may not have the need to undergo sex change surgery or even begin living in their preferred gender.
Genital procedures like penectomy and orchidectomy, vaginoplasty and clitorolabioplasty in male-to-female transsexuals, are the core procedures done in gender reassignment surgery. Nongenital procedures like breast augmentation, facial feminization surgery andtracheal shave procedures complete the surgical treatment available
A candidate opting for sex reassignment surgery should fill up these criteria for Hormonal therapy or Breast/non genital Surgery
- Patient must be a major, above the age of 18 years (or Parental release form).He or she should have capacity to make a fully informed decision and to consent for treatment.
- Must be in stable frame of mind, and are living in society as the new desired external appearance (Real Life Experience) for at least 3-months.
- Persistent, well-documented gender dysphoria
- Consultation & counselling with psychiatrist (mental health physician) for at least 3-months, to rule out any abnormal mental status or infatuation or temporary attraction/any secondary gain; and approval of psychiatrist to undergo hormonal therapy and/or breast surgery.
- Affidavit (notarized) from patient that he/she is major and can fully understand pros/cons & take the decision regarding the therapy/surgery.
A candidate opting for sex reassignment surgery should fill up these criteriafor Genital Surgery
- Patient must be a major, above the age of 18 years (or Parental Release Form) He or she should have capacity to make a fully informed decision and to consent for treatment.
- If married, the spouse must sign Spousal Release Form
- Persistent, well-documented gender dysphoria
- Must be in stable frame of mind, and are living in society as the new desired external appearance (Real Life Experience) for at least 1-year.
- Continuous consultation & counselling with psychiatrist (mental health physician) for at least 1-year; and approval with two independent Psychiatrists for surgery at two different intervals (a gap of at least 6-months) to rule out any abnormal mental status or infatuation or temporary attraction and IQ of patient.
- Affidavit (notarized) from patient that he/she is a major and can take decisions regarding the surgery after fully understanding the pros & cons and understanding of irreversibility of the procedures.
Discussions during a Male-to-female sex reassignment surgery consultation should include
- Discussion on the body/genital/face reshaping goals.
- Sequence of genital and non-genital surgeries.
- Any past medical condition or surgeries.
- Any present illness, drug allergies and medical treatments.
- Any on-going supplements
- Alcohol, tobacco and drug use
Dr Amit Agarwal's focus during Male-to-female sex reassignment surgery consultation
- Examine your overall health, mental status, and risk factors
- Discuss the options for your MTF transition.
- Take photographs
- Risk and complications related to different surgical procedures involved in the transition
- Outcome of surgery
- Hormone therapy to be tapered off–especially oestrogen—for a couple of weeks before surgery to reduce the risk of blood clots
Questions to be asked with Dr Amit Agarwal aboutMale-to-female sex reassignment surgery
- What happens during transgender surgery?
- How and where will you perform the surgery?
- What are the risks and complications related to the surgery?
- How long will be my recovery period?
- How long do I have to stay in the hospital?
Preparations to be done for the surgery
- Stop smoking at least 2 weeks prior to surgery.
- Do not take any anti-inflammatory drugs, aspirin or any herbal supplements as they can aggravate bleeding.
- Written consent form will be signed explaining the procedure after the admission.
- Nil per oral for minimum of 5-6 hours before the planned procedure.
- Refrain from drinking alcohol 48 hours before the surgery, since it can affect the anaesthesia
Male-to-female sex reassignment surgery procedure includes
Genital Surgery
The genital surgeries include two distinct procedures: removing male sex organs-the testes and the penis, and the creation of female sex organs - vagina, labia and clitoris.
Removing Male sex organs - testicles, penis
Surgical removal of the testicles can be done before the penis is removed to allow the patient to reduce the intake of female hormones. Because the testes are the main producers of the male hormone testosterone, removing them also reduces the amount of oestrogen the patient needs to take and thus reduces the risks associated with oestrogen.Testes are encased in a skin pouch, the scrotum. During testis removal, scrotum skin is left behind to be used in creating the labia or to line part of the vagina during vaginoplasty.
Surgical removal of the penis is done after itcreating a shallow vaginal dimple and a new urethral opening to allow for urinating in a sitting position. The genital part of the sex change surgery can stop with it without creation of female genitals. When done without vaginoplasty, a penectomy is called nullification. Patients who are not sure they want a vagina will stop with just removal of penis and testes. If female genitalia have to created, penile skin and tissue from head will be preserved to be fashioned into a vagina and clitoris.
Creation of the female genitals
Creating female genitals entails vaginoplasty, labiaplasty and clitoroplasty. Vaginoplasty is the creation of a vagina. Labiaplasty refers to the creation of labia, and clitoroplasty, the creation of the clitoris.
It is necessary to preserve your ability to have orgasms, to create a clitoris, labia, and an opening to the vagina that both look good and feel good when touched.
Vaginoplasty - You should make your expectations clear to your surgeon before vaginoplasty surgery. Ideally, the created vagina should be able to retain its shape, be sensitive to touch and be sufficiently wide and long enough for sexual penetration. The new vagina should also be moist and elastic, with a hairless lining. Another goal of vaginoplasty is to change the structure of the urinary tract to enable urinating downwards and in a steady stream.All the mentioned points are difficult to achieve in all cases.
- Penile inversion is the most common technique used in vaginoplasty. The technique uses the skin of the penis turned inside out to line walls of the new vagina. Extra skin needed to make the vagina wider and longer is usually taken from the scrotal sac.
- If it is important to you that the vagina be long and wide enough for penile penetration, it may be necessary to have skin grafts from the thigh region. This is usually done where the penile skin is too small for creating an adequately sized vagina.
- If penis was damaged or removed earlier, vagina can be created with the skin graft harvested from the thigh or with a segment of the large intestine as the vaginal lining.
Clitoroplasty - The clitoris is created using a small section of the highly sensitive penis head. The erectile tissue, which gave the penis the ability to become erect, is removed in order to prevent the vagina entrance and the clitoris from becoming overly swollen during sexual arousal.
Urethroplasty - The urethra, a tube that carries urine from the bladder to outside the bodyis found in a different position in females than in males. It is also much longer in biological males than in females. During vaginoplasty, the urethra is shortened and repositioned.The prostate gland, which is found at the neck of the bladder and around the urethra, is not removed during vaginoplasty.
Labiaplasty - The labia minora, the innermost lips of the vagina, are typically fashioned from leftover penis skin if present. Labia majora, the outer labia, are created using the skin of the scrotum.
Non-genital surgeries
Non genital surgeries can be staged and done after 6 months of genital surgery or vice versa. A more practical approach followed is to do non genital surgery firstas they are reversible and then do the genital surgeries after 6 months to one year of non genital surgery.
Facial feminization surgery - include procedures that modify bone structures, typically in the lower jaw, brow region, forehead and cheek areas and cartilage structure of nose to soften the facial features. Typically surgery is done through areasso that no scars are visible on the skin.
Breast augmentation - Breast augmentation is the enlargement of the breasts with silicone prosthesis. This surgery is usually chosen as the first surgery by most MTF individuals as it is most satisfying and give immediate results with social approval. Oestrogen is responsible for fat distribution to the breasts, hips and buttocks, while progesterone is responsible for developing the actual milk glands. Progesterone also rounds out the breast to an adult Tanner stage-5 shape and matures and darkens the areola.
Voice feminization surgery - Someindividuals may elect to have voice surgery, which alters an individual's vocal range or pitch. However, this procedure carries a risk of impairing a trans woman's voice forever. Since estrogen alone does not alter a person's vocal range or pitch, some people take the risk that comes along with voice feminization surgery. Other options, like voice feminization lessons, are available to people wishing to speak with less masculine mannerisms.
Tracheal shave - A tracheal shave procedure is also sometimes used to reduce the cartilage in the area of the throat and minimize the appearance of the Adam's apple.
Buttock augmentation - Some individuals will choose to undergo buttock augmentation because anatomically, male hips and buttocks are generally smaller than those presented on a female
Recovery after the surgery
You will be closely monitored as you come out of the anaesthesia. It is necessary to stay in hospital until you are sufficiently recovered to go home. After non genital surgery, you will be sent back home next day after surgery.After genital surgery, usually this is about six to eight days after surgery, unless only testes removal was done. Both penectomy and vaginoplasty are serious surgeries and need longer recovery periods.
- During the early stages of recovery, you will be restricted to bed rest and on injectable pain killers, antibiotics and anticoagulants to help prevent blood clots.
- Following vaginoplasty, a rod-shaped prosthesis will be placed in your vagina. It will be left in place for up to five days to help the skin lining your new vagina properly attach itself to the vaginal wall. A catheter will be placed in the new urethra to drain urine from your bladder. Both of these will be removed about five days after surgery to enable the surgeon to see how you are healing.
- By the second week you will start to feel more comfortable physically, but your recovery will take a long time. It is natural to experience pain and soreness for a long time after genital surgery.
- Surgical incisions will be monitored for scarring and infection. Your bowel movements and bladder function will be monitored.
- If a newly created vagina is not dilated every day after surgery, it may become shorter and narrower than you wish it to be. This is why for the first 3 months following vaginoplasty you will be asked to wear a prosthesis inside the vagina at all times. At first you will take it out once a day to clean it, and the period of time you leave it out will gradually increase.To keep your vagina open, you will still need to continue to dilate it every day. Otherwise, over time the vagina may become narrow and short.
- Most people feel well enough to get back to their usual routines within four to six weeks. By this time, normal movement should not cause any pain. In some cases, healing takes longer.
- It is important to avoid rigorous activity or excercise until full recovery.
- Testes removal puts an end to most of your testosterone production, but once you feel well enough to resume light activities, oestrogen therapy will resume again, tailored to your specific needs.
- It is important to work with a physician to ensure you are taking an appropriate dose of hormones after your surgery. If you would prefer not to take oestrogen, it is necessary to substitute another type of medication to prevent loss of bone density. Without proper hormone treatments, trans people can be at risk of osteoporosis.
Risk and complications post-surgery
Before going for the surgery, you should always understand the risks and potential complications related to surgery. Non genital surgery like breast augmentation can have few risks which can be read in the section by clicking on the link. Male-to-female sex reassignment surgery usually gives desired results but there can be some risks involved with genital surgery which include:
- Risks related to anaesthesia.
- A drop in sexual sensation and possibly a decrease in the ability to have an orgasm. This is a potential long-term risk of vaginoplasty. Various studies report the ability to have an orgasm following vaginoplasty in male to female transition within the range of 63 percent to 94 percent. Some transwomen however, have reported an inability to orgasm after surgery.
- There can be persistent swelling and bruising in the surgical area which reduces with time.
- If you have a poor blood supply, the healing will be poor.
- Irregular pigmentation of the surgical area.
- Rupture of multiple stitches that open up the wound.
- Narrowing or closure of the new vagina, which you will experience as difficulty or pain during vaginal penetration
- Narrowing or closure of the restructured urethra, causing difficulty in urinating, painful urination or a significant reduction in the amount of urine excreted. If you experience any of this, or find that you need increased time and effort to urinate, tell the surgeon without delay.
These are the risks and possible complication which should be discussed by you with your surgeon before the procedure.
Frequently Asked Questions
Male to female sex change operations are for people who are biologically male, but who identify as women and wish to live their lives as women.
Male to female sex change surgery involves multiple operations, both genital and non genital.
Many transgender individuals choose to undergo fertility preservation before their gender affirmation surgery if having biological children is part of their long-term goals.
This procedure is performed under regional or general anaesthesia. During the procedure you will not feel any pain but there may be some pain and swelling during the recovery process.
Quitting smoking is a perfect solution even without surgery as it involves many health risks, but it's totally up to your wish that you want to quit or not. But you should surely stop smoking at least 2 weeks before the surgery.
Research has shown that transgender individuals who choose gender-affirming surgery experience long-term mental health benefits. In one study, a person's odds of needing mental health treatment declined by 8% each year after the gender-affirming procedure.
Male to Female Images
Indivisual results may vary from person to person.
These pictures are shown for the purpose of education only.


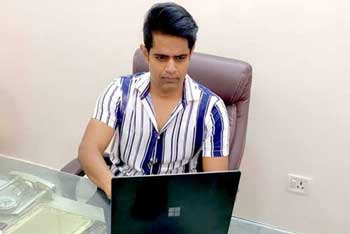
Know your surgeon better

Best plastic surgeon, Dr. Amit Agarwal is an American Board Certified, extensively trained, and best Plastic & Aesthetic surgeon in Lucknow. He is the Chief Plastic Surgeon heading the Department of Plastic, Microvascular, and Craniofacial surgery at Vivekananda Polyclinic and Institute of Medical Sciences, Lucknow, U.P, India. He maintains a busy practice at Avadh and Nishat Hospital and his own center - Kayakriti Plastic Surgery & Dental Center. He was formerly a Consultant in the Department of Plastic Surgery and Burns at the prestigious SGPGI, Lucknow.
MS, DNB (General Surgery) MCh, DNB (Plastic Surgery),
MNAMS, FACS, FICS, FRCS (Edinburgh, UK)
His Credentials
Three pillars of kayakriti
Privacy
We believe your experience with us should be comfortable and hassle-free to make it one of your best lifetime experiences for yours. We, here at the clinic, take full precautions to maintain your privacy in any manner. We also provide a staff who will receive you from the gate and take you to the chamber directly if you demand.
Trust
Our Surgeon is highly qualified and internationally certified with a team of skilled staff to perform any surgical or non-surgical treatment on your body.
Safety
When you plan to undergo any surgery you should always keep in mind that it's your body and it's a surgery. We, here always keep your safety a priority and will never recommend you to undergo any such procedure which is not safe for you. We also provide you with a detailed description of the complications which may occur after the surgery during the consultation as it's a surgical procedure so there may be some complications depending on the way your body reacts.
Kayakriti in news



Frequently Asked Questions
If you have flat or small breast and you want to improve your breast and hip contour ratio then you are a good candidate for it. The answer will be best provided after the first consultation with Dr Amit Agarwal.
Acute pain will be there for almost a week which gradually reduces and there will be soreness and swelling which may take up to 3 weeks to subside.
You can join your work and daily routines after a week of the procedure and can start exercising after 3 weeks of it.
Yes, you have to wear it round the clock unless we suggest you to remove it.
This surgery does not affect the ducts or the areas of the breast involved in milk production. Thus, it does not affect the breast feeding.
This surgery does not affect the ducts or the areas of the breast involved in milk production. Thus, it does not affect the breast feeding.











Kayakriti Plastic Surgery & Dental Center
D-43, Near Punjab National Bank, Rajajipuram, Lucknow, Uttar Pradesh - 226017, India
Phone No. +919695940009, +919695940006
Map Location





















Social Media Presence