Female to Male
gender reassignment surgery
Gender reassignment treatment has been demonstrated as the most effective treatment for patients affected by gender dysphoria.

Gender reassignment treatment (which includes psychotherapy, hormonal therapy and surgery) has been demonstrated as the most effective treatment for patients affected by gender dysphoria (or gender identity disorder), in which patients do not recognize their gender (sexual identity) as matching their genetic and sexual characteristics.
Gender dysphoria, also known as transgenderism or gender identity disorder (GID), is a condition in which a person feels a major mismatch between their biological sex and their gender identity. It is not a type of mental illness, although it was wrongly believed to be one in the past.
People with gender dysphoria can be treated with counselling, hormone therapy and sex change surgical procedures. Not every transgender individual requires or wishes to undergo sex change surgery. Some are treated with counselling only; others may get counselling and/or hormone therapy. But some trans people do end up going through sex change operations.
Sex change surgery is irreversible. Therefore (and obviously) anyone wishing to undergo a sex change operation from female to male should carefully consider that decision.
Sex change surgery is a series of complex surgical procedures (genital and non-genital) performed for the treatment of gender dysphoria. Female-to-male sex reassignment surgery involves reshaping the female genitals into a form with the appearance of, and as far as possible, the function of male genitalia.
Sex change surgery usually follows hormone therapy. It is necessary to have a letter from a psychiatrist before a physicianbegins hormone therapy.
A patient must be over 18 years and understand what hormones can and cannot do medically. It is also necessary to understand the social benefits and risks of hormone therapy. A minimum of three months of psychotherapy or a documented three-month real-life experience is necessary to be eligible for hormone therapy. FTM people should have stable mental health and demonstrate their ability to take hormones in a responsible manner to be started on hormone therapy by a physician.
For FTM's hormone therapy involves taking the male hormonetestosterone taken orally or by injection. It will be necessary during all stages of the transition, before, during and after the sex change surgeries. Hormone therapy in female to male transition is important because it helps change the physical appearance to resemble a man more closely.
For some people, all the treatment they need to treat transgenderism is hormone therapy. Because hormones affect the way they feel, they may not have the need to undergo sex change surgery or even begin living in their preferred gender.
Genital procedures like removal of uterus and ovaries, phallus reconstruction or metaidoioplasty and scrotal reconstruction in female-to-male transsexuals, are the core procedures done in gender reassignment surgery. Non genital procedures like breast removal, facial and body masculinization surgery procedures complete the surgical treatment available
A candidate opting for sex reassignment surgery should fill up these criteria for Hormonal therapy or Breast/ non genital Surgery
- Patient must be a major, above the age of 18 years (or Parental release form). He or she should have capacity to make a fully informed decision and to consent for treatment.
- Must be in stable frame of mind, and are living in society as the new desired external appearance (Real Life Experience) for at least 3-months.
- Persistent, well-documented gender dysphoria
- Consultation & counselling with psychiatrist (mental health physician) for at least 3-months, to rule out any abnormal mental status or infatuation or temporary attraction/any secondary gain; and approval of psychiatrist to undergo hormonal therapy and/or breast surgery.
- Affidavit (notarized) from patient that he/she is major and can fully understand pros/cons & take the decision regarding the therapy/surgery.
A candidate opting for sex reassignment surgery should fill up these criteriafor Genital Surgery
- Patient must be a major, above the age of 18 years (or Parental Release Form) He or she should have capacity to make a fully informed decision and to consent for treatment.
- If married, the spouse must sign Spousal Release Form
- Persistent, well-documented gender dysphoria
- Must be in stable frame of mindand are living in society as the new desired external appearance (Real Life Experience) for at least 1-year.
- Continuous consultation & counselling with psychiatrist (mental health physician) for at least 1-year; and approval with two independent Psychiatrists for surgery at two different intervals (a gap of at least 6-months) to rule out any abnormal mental status or infatuation or temporary attraction and IQ of patient.
- Affidavit (notarized) from patient that he/she is a major and can take decisions regarding the surgery after fully understanding the pros & cons and understanding of irreversibility of the procedures.
Discussions during a Female-to-male sex reassignment surgery consultation should include
- Discussion on the body/genital/face reshaping goals.
- Sequence of genital and non-genital surgeries.
- Any past medical condition or surgeries.
- Any present illness, drug allergies and medical treatments.
- Any on-going supplements
- Alcohol, tobacco and drug use
Dr Amit Agarwal's focus during Female-to-male sex reassignment surgery consultation
- Examine your overall health, mental status, and risk factors
- Discuss the options for your FTM transition.
- Take photographs
- Risk and complications related to different surgical procedures involved in the transition
- Outcome of surgery
Questions to be asked with Dr Amit Agarwal aboutFemale-to-male sex reassignment surgery
- What happens during transgender surgery?
- How and where will you perform the surgery?
- What are the risks and complications related to the surgery?
- How long will be my recovery period?
- How long do I have to stay in the hospital?
Preparations to be done for the surgery
- Stop smoking at least 2 weeks prior to surgery.
- Do not take any anti-inflammatory drugs, aspirin or any herbal supplements as they can aggravate bleeding.
- Written consent form will be signed explaining the procedure after the admission.
- Nil per oral for minimum of 5-6 hours before the planned procedure.
- Refrain from drinking alcohol 48 hours before the surgery, since it can affect the anaesthesia
Female-to-male sex reassignment surgery procedure includes
Each FTM has his own unique needs and expectations, which is why we take an individualized, patient-centred approach to gender transition services. During the preoperative consultation, Dr Amit Agarwal will take the time to discuss and understand your goals for gender transition. Additionally, he'll thoroughly explain each procedure and answer any questions you might have.
Non-genital surgeries
Non genital surgeries can be staged and done after 6 months of genital surgery or vice versa. A more practical approach followed is to do non genital surgery first as they are reversible and then do the genital surgeries after 6 months to one year of non-genital surgery.
Breast removal - This surgery is usually chosen as the first surgery by most FTM individuals as it is most satisfying and give immediate results with social approval. Mastectomy to remove the breasts is the most gratifying surgery for FTM individuals and is a very safe and commonly performed procedure. Alterations in the nipple and areola size and shape is also done along with the breast removal. Every case of FTM breast removal is different and requires a discrete and different approach in every case to achieve the desired aesthetic result. These include bilateral mastectomy with free nipple grafts, the peri-areolar/keyhole technique, and adjunctive lateral chest wall liposuction. With the help of testosterone therapy, chest hair grows.
Facial masculinization surgery - are procedure done to give a more chiselled and masculine appearance to the face. Because facial features offer important visual cues as to one's gender, FMS is a vitally important aspect of the FTM transition. Each FTM will have different goals and needs. Therefore, Dr Amit Agarwal will work with you to design a customized surgical plan.
- Forehead lengthening/augmentation,
- Male Rhinoplasty,
- Chin recontouring and Jaw contouring, and
- Thyroid cartilage enhancement (Adam's Apple surgery)
Body Masculinization Surgery - is for the transman who would like to achieve a more masculine contour throughout the upper and lower body. The traditional male body includes a broad and defined upper torso, trim waist, and minimal fat in the lower body area. While diet, exercise, and hormone therapy play a role in masculinizing the body, certain areas of fat storage can be difficult to change without surgery. BMS is a liposuction technique that targets fat in the flanks, inner and outer thighs, upper body, chest, back, and/or buttocks to reduce the feminine "hourglass" shape and create a masculine physique. Liposuction is a safe and minimally invasive procedure.
Voice masculinisation surgery - Some individuals may elect to have voice surgery, which alters an individual's vocal range or pitch. This surgery is done by an ENT specialist. However, this procedure carries a risk of impairing a trans man's voice forever. Other options, like voice lessons, are available to people wishing to speak with more masculine mannerisms.
Genital Surgery
The genital surgeries include two distinct procedures: removing female sex organs-uterus and ovaries, and the creation of female sex organs–phallus and scrotum.
Removing Female sex organs – Uterus and ovaries - Removal of uterus, ovaries & the fallopian tubes is advised only if the patient is willing to remove them or if even after the testosterone therapy menstruation doesn't stop. The procedure done is hysterectomy and Bilateral Salpingo-oophorectomy (Removal of Uterus, bilateral fallopian tubes & ovaries. Surgical removal of female gonads is done to allow the patient to reduce the intake of male hormones. Because the ovaries are the main producers of the female hormone testosterone, removing them also reduces the amount of testosterone the patient needsto take and thus reduces the risks associated with testosterone.
Creation of the Male genitals - You should make your expectations clear to your surgeon before phallus surgery. Ideally, the created phallus should be aesthetically appealing, with erogenous and tactile sensation, which enables the patient to void while standing and have sexual intercourse like a natural male. The reconstructive procedure should also provide a normal scrotum, be predictably reproducible without functional loss in the donor areaand leave the patient with minimal scarring or disfigurement. All the mentioned points are difficult to achieve in all cases.
1) Penile Reconstruction with flap technique - Vaginectomy, urethral reconstruction, scrotoplasty and phalloplastyis done by two simultaneously operating surgical teams with the patient first placed in a gynecological (lithotomy) position. A vaginectomy, pelvic floor reconstruction and lengthening of the urethra is done between the labia minora. This is followed by scrotal reconstruction by means of two transposition flaps of the labia majora resulting in a very natural looking bifid scrotum. The created scrotal sac is inserted with silicone testicular implants.
Simultaneously, radial forearm free flap is harvested from forearm or Anterolateral thigh flap from thigh to reconstruct phallus. RAFFF from forearm is universally considered the gold standard in penile reconstruction. A penis with a tube-in-a-tube technique is created, the urethra is lengthened and the acceptor (recipient) vessels are dissected in the groin area. The patient is put into a supine position and free flap is transferred to the pubic area. Urethral anastomosis and artery, veinaremicrosurgically connected to the vessels in the groin. One forearm nerve is connected to the ilioinguinal nerve for protective sensation and the other nerve of the arm is anastomosed to one of the dorsal clitoral nerves for erogenous sensation. The clitoris is usually denuded and buried underneath the penis, thus keeping the possibility to be stimulated during sexual intercourse with the neophallus. The defect on the forearm was covered with full-thickness skin grafts taken from the groin area or thick SSG from thigh region.
After complete recovery of 3 months, Penile Implants can be placed to maintain erections & have penetrative sex.
Points to remember in Penile reconstruction
- Phalloplasty helps to create a larger penis, but with a disadvantage of this new penis not becoming erectile on its own.
- It requires large number of surgical visits.
- The procedure costs more than Metoidioplasty.
2) Metoidioplasty - Metoidioplasty involves the change of clitoris into a penis for which the clitoris receives hormone therapy to enlarge its size. A metoidioplasty uses the (hypertrophied) clitoris to reconstruct the new small penis in a way comparable to the correction of chordee and lengthening of a urethra in cases of severe hypospadias. In metoidioplasty, the clitoral hood is lifted and the suspensory ligament of the clitoris is detached from the pubic bone, allowing the clitoris to extend out further. An embryonic urethral plate is divided from the underside of the clitoris to permit outward extension and a visible erection. Then the urethra is advanced to the tip of the new penis. During the same procedure, a scrotal reconstruction, with a transposition flap of the labia majora (as previously described) is done combined with a vaginectomy.
Points to remember in Metoidioplasty
- There will be no scars outside the genital region
- Due to the erectile capacities of clitoral tissues, the new penis has chances of becoming erect.
- Voiding while standing cannot be guaranteed
- Sexual intercourse will not be possible as the penile length will not be long enough.
Penile reconstruction with flap (e.g., with a radial forearm flap) cane be done at a later stage also after metoidioplasty, and with substantially less risk of complications and operation time.
Recovery after the surgery
You will be closely monitored as you come out of the anaesthesia. It is necessary to stay in hospital until you are sufficiently recovered to go home. After non genital surgery, you will be sent back home next day after surgery. After chin, nose and jaw surgery: Most swelling fades within 2-3 weeks. After Breast removal: Swelling and soreness last for two weeks. Avoid vigorous activity for at least one month.
After genital surgery, you will be sent home usually about 10-14 days after surgery,
- During the early stages of recovery, you will be restricted to bed rest and on injectable pain killers, antibiotics and anticoagulants to help prevent blood clots.
- All patients receive a suprapubic urinary diversion after surgery.
- All patients remain in bed during a two-week postoperative period, after which the transurethral catheter is removed. At that time, the suprapubic catheter is clamped, and voiding of urine from new penisis begun. Effective voiding might not be observed for several days. Before removal of the suprapubic catheter, a cystography with voiding urethrography is performed.
- The average hospital stay for the phalloplasty procedure is 10–14 days.
- By the second week you will start to feel more comfortable physically, but your recovery will take a long time. It is natural to experience pain and soreness for a long time after genital surgery.
- Surgical incisions will be monitored for scarring and infection. Your bowel movements and bladder function will be monitored.
- Most people feel well enough to get back to their usual routines within four to six weeks. By this time, normal movement should not cause any pain. In some cases, healing takes longer.
- It is important to avoid rigorous activity or exercise until full recovery.
- Tattooing of the glans can be done after 3-months of surgery, before sensation returns to the penis.
- Implantation of the testicular prostheses can be done after 6 months also (if not done along with surgery, but it is typically done in combination with the implantation of a penile erection prosthesis. Sensation must be returned to the tip of the penis before implants are used. This usually does not occur for at least a year.
It's important to understand that, for most people, surgery is only one part of the transitioning process. After surgery, one should continue to work with a therapist or counsellor as they can support with social transitioning and your mental health.
Risk and complications post-surgery
Before going for the surgery, you should always understand the risks and potential complications related to surgery. Non genital surgery like breast removal, chin, jaw, nose surgery can have few risks which can be read in the section by clicking on the link. Female-to-male sex reassignment surgery usually gives desired results but there can be some risks involved with genital surgery which include:
- Risks related to anaesthesia. General Anaesthesia is very safe in present times and with best machines and a qualified anaesthetist, chances of encountering any complication are less than 0.1 percent in a healthy individual. But no one can predict who will land up in complication. We at Kayakriti Plastic Surgery and Dental Centre are equipped with world class anaesthesia workstation, other equipments and two very qualified intensivists for the surgical procedures to be very safe and smooth.
- There can be persistent swelling and bruising in the surgical area which reduces with time.
- Risks related to higher BMI like medical condition or higher the BMI, higher are the risks.
- Seroma formation or fluid accumulation can be there which usually deceases with time.
- Rare chances of infection which responds to prolonged antibiotic therapy.
- Bleeding or haematoma formation can occur which might require drainage.
- Poor wound healing because of poor blood supply of flaps. Seen more commonly in smokers, diabetes, hypothyroidism and individuals with multiple comorbidities. Poor wound healing can lead to skin discoloration which can cause marginal or total skin necrosis
- Numbness or altered skin sensation over the created chest region.
- Scars will be there along the incision line which will fade with time. Scars can get hypertrophied if you are prone for it.
- Rare event of Deep vein thrombosis, pulmonary or cardiac complications can occur or precipitate in patients with multiple pre-existing diseases diagnosed or undiagnosed by routinely available standard tests. It can occur in FTM patients despite adequate preventive measures.
- Possibility of revision surgery.
Complications specific tometoidioplasty procedure include urethral obstruction and/or urethral fistula.
Breast removal complications include bleeding (most frequent, despite drains and compression bandages), (partial) nipple necrosis, and abscess formation. Skin slough of the NAC can also happen which can be left to heal by conservative means. Rare complication of Total nipple necrosis may require a secondary nipple reconstruction. Even in the patients without complications, ~25% required an additional procedure to improve the aesthetic results of their chest region in future.
Complications of Penile Reconstruction - For FTM, the ability to void while standing is a high priority. Unfortunately, the reported incidences of urological complications, such as urethrocutaneous fistulas, stenoses, strictures, and hairy urethras are high. Most complications of the radial forearm phalloplasty are related to the free tissue transfer. The whole flap can fail and would require an additional surgery. Risks related to Microsurgical reconstruction of flap technique like thrombosis or blood clot in the vessels of the flap, re-exploration/re-surgery to remove these clots, and flap failure is seen in less than 5 percent of cases. Few patients develop some degree of skin slough or partial flap necrosis. This was more often the case in smokers, in those who insisted on a large-sized penis requiring a larger flap, and also in patients having undergone anastomotic revision.
These are the risks and possible complication which should be discussed by you with your surgeon before the procedure.
Frequently Asked Questions
Female to male sex change operations are for people who are biologically female, but who identify as male and wish to live their lives as a man.
Female to male sex change surgery involves multiple operations, both genital and non-genital.
Many transgender individuals choose to undergo fertility preservation before their gender affirmation surgery if having biological children is part of their long-term goals.
This procedure is performed under general anaesthesia. During the procedure you will not feel any pain but there may be some pain and swelling during the recovery process.
Quitting smoking is a perfect solution even without surgery as it involves many health risks, but it's totally up to your wish that you want to quit or not. But you should surely stop smoking at least 2 months before the surgery.
Research has shown that transgender individuals who choose gender-affirming surgery experience long-term mental health benefits. In one study, a person's odds of needing mental health treatment declined by 8% each year after the gender-affirming procedure.
Female to Male Images
Indivisual results may vary from person to person.
These pictures are shown for the purpose of education only.


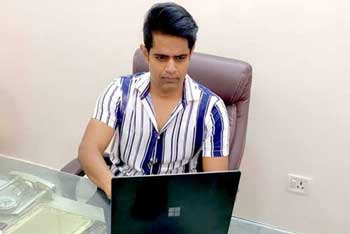
Know your surgeon better

Best plastic surgeon, Dr. Amit Agarwal is an American Board Certified, extensively trained, and best Plastic & Aesthetic surgeon in Lucknow. He is the Chief Plastic Surgeon heading the Department of Plastic, Microvascular, and Craniofacial surgery at Vivekananda Polyclinic and Institute of Medical Sciences, Lucknow, U.P, India. He maintains a busy practice at Avadh and Nishat Hospital and his own center - Kayakriti Plastic Surgery & Dental Center. He was formerly a Consultant in the Department of Plastic Surgery and Burns at the prestigious SGPGI, Lucknow.
MS, DNB (General Surgery) MCh, DNB (Plastic Surgery),
MNAMS, FACS, FICS, FRCS (Edinburgh, UK)
His Credentials
Three pillars of kayakriti
Privacy
We believe your experience with us should be comfortable and hassle-free to make it one of your best lifetime experiences for yours. We, here at the clinic, take full precautions to maintain your privacy in any manner. We also provide a staff who will receive you from the gate and take you to the chamber directly if you demand.
Trust
Our Surgeon is highly qualified and internationally certified with a team of skilled staff to perform any surgical or non-surgical treatment on your body.
Safety
When you plan to undergo any surgery you should always keep in mind that it's your body and it's a surgery. We, here always keep your safety a priority and will never recommend you to undergo any such procedure which is not safe for you. We also provide you with a detailed description of the complications which may occur after the surgery during the consultation as it's a surgical procedure so there may be some complications depending on the way your body reacts.
Kayakriti in news



Frequently Asked Questions
If you have flat or small breast and you want to improve your breast and hip contour ratio then you are a good candidate for it. The answer will be best provided after the first consultation with Dr Amit Agarwal.
Acute pain will be there for almost a week which gradually reduces and there will be soreness and swelling which may take up to 3 weeks to subside.
You can join your work and daily routines after a week of the procedure and can start exercising after 3 weeks of it.
Yes, you have to wear it round the clock unless we suggest you to remove it.
This surgery does not affect the ducts or the areas of the breast involved in milk production. Thus, it does not affect the breast feeding.
This surgery does not affect the ducts or the areas of the breast involved in milk production. Thus, it does not affect the breast feeding.











Kayakriti Plastic Surgery & Dental Center
D-43, Near Punjab National Bank, Rajajipuram, Lucknow, Uttar Pradesh - 226017, India
Phone No. +919695940009, +919695940006
Map Location





















Social Media Presence